Have you seen a surgeon and been told you have a disc prolapse? Maybe you have googled around and self-diagnosed it? Or have you got ‘sciatica’ and want to know more?
At Complete Pilates we see thousands of people with problems just like these.
Meet Mr Alexander Montgomery. Below, he is answering all the questions we hear on a daily basis in the studio and online! Remember, if you want to know more just ask us.
We are trying to make your rehabilitation and treatment as clear as possible so have put together this patient information handout. Please feel free to contact us if you have any questions.
What is a disc prolapse?
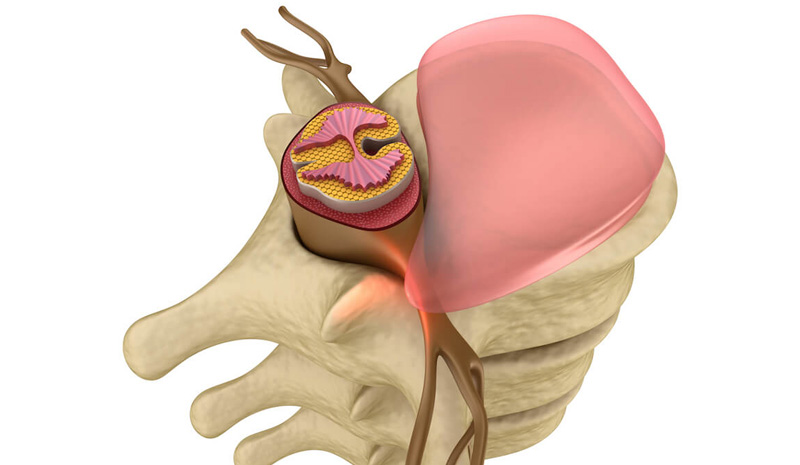
It is first important to understand the anatomy. The discs in your spine sit between the bones and work like a cushion. Inside these discs is a gel-like substance. This enables them to act as shock absorbers and prevent damage to the bones and joints as you move around.
A disc prolapse is when some, or all, of the gel-like contents of the disc come out and go into the spinal canal. This can cause none, or a variety of symptoms which we will discuss later.
Is a disc prolapse and bulging disc the same thing?
Fundamentally no. A disc prolapse is when the gel-like substance within the disc comes through the outer layer (annulus) through a small tear and into the spinal canal. However, a disc bulge is when there is no tear and the disc pushes out to occupy more space than it normally would.
Should I be worried about having a disc bulge?
In short, no. A disc bulge is very common, with most causing little or no symptoms. If they do cause you symptoms, most settle down naturally over 4-8 weeks or with physiotherapy, or appropriate one to one Clinical Pilates. However, some do take longer to settle and a small percentage of them cause persistent problems. This is when you should seek a referral to a Consultant.
How common is a disc bulge?
Disc bulges are very common. They are more common in men than women and particularly occur in people aged between 30 and 50 years old. By the age of 40, 40% of people with no symptoms will have a disc bulge shown on MRI. This can be considered as normal age-related change and occurs from as early as our late teens or early 20’s.
Approximately 95% of disc prolapses which occur in people aged 25-55 are in the lumbar spine.
Can my disc prolapse heal?
Discs do not heal as such. When you have a disc prolapse or ‘slipped disc’, the body will see this as foreign material. Consequently, you develop an inflammatory response. This attracts chemicals to the area which dissolve the part of the disc that has prolapsed. This happens over a period of weeks or months. When the inflammatory reaction occurs, it can be painful, but in most people begins to settle over 2-8 weeks.
What are the symptoms of a slipped disc?
As we have already talked about, prolapsed or ‘slipped’ discs, can be symptom free and are part of normal age-related changes. However, if you are getting symptoms, they can include the following:
Lumbar spine (lower back):
- Pain that radiates to the buttocks, legs, and feet. Most people recognise this as ‘sciatica’. With this you may or may not also have back pain.
- Pins and needles or numbness in the legs or feet.
- Muscle weakness in the lower limb.
- Back spasm or pain.
If you have leg pain with incontinence, problems going to the toilet, numbness in your saddle area or problems walking due to numbness and weakness it may be an emergency, so it is advised you go immediately to A&E.
Cervical spine (neck):
- Pain near or over the shoulder blade which may also present as a tightness or discomfort.
- Pain which radiates to the shoulder, arm and sometimes hand and fingers.
- Pins and needles and numbness in the arm or hands.
- Weakness in the arm or hands.
- Neck pain particularly around the back and sides.
- Spasm in the neck muscles.
If you have problems with balance or walking which is associated with your neck and arm symptoms, you should consult your doctor immediately. This may indicate spinal cord compression in the neck.
Am I more likely to have another disc prolapse if I have one already?
Disc degeneration is completely normal. The speed at which this happens is mainly related to your genetics. A family history of disc prolapses may mean that you are at risk of accelerated degeneration and consequently disc prolapses. However, there are other factors.
Smoking is the second biggest cause. This is followed by other lifestyle factors such as heavy weight lifting and occupational factors.
Continually lifting heavy weights with poor technique results in there being a greater probability of experiencing another disc problem. If you also have a history of repetitive impact or contact sport, such as running or rugby, it may also put you at increased risk.
If you are overweight it can cause increased stress on your discs, particularly in the lower back. Occupations which involve repetitive lifting and twisting or prolonged sitting, particularly if you sit with poor posture, can also put you at a higher risk of pain.
What happens in a discectomy?
A discectomy is an operation to remove part, or sometimes all, of the disc which is compressing a nerve. It is done when a patient has not got better with physiotherapy, appropriate one to one Pilates, or injections. It may also be recommended to you if you have progressive weakness in the limb, or in an emergency when there are problems with incontinence or going to the toilet.
In a lumbar discectomy, a small incision is made in your back, the muscles are retracted, and small portions of ligament is removed. The correct nerve is identified and carefully retracted so that the protruding disc can be removed. Sometimes, small portions of bone need to be removed but this does not affect the stability of your spine.
In a cervical discectomy, a small incision is made at the front of your neck. The structures in your neck are retracted and the disc removed. An implant is inserted in its place. This is normally a cage or disc replacement.
Do you take away the whole disc in a discectomy?
Normally only the part of the disc which is compressing the nerve is removed. However, you should check with your surgeon prior to your operation what they are likely to do.
Will I get an arthritic spine after a discectomy?
In all of us the discs and joints naturally wear down with time. How quickly this occurs is primarily determined by your genetics. If you have a diagnosed disc prolapse at one or more levels, these levels are likely to wear down quicker than other levels.
Seeing signs of ‘wear and tear’ (degeneration or arthritis) in your MRI scan does not mean you will experience pain. Often this is normal, and people are still pain free. However, when looking at the longer-term picture, it is important to participate in activity which will encourage flexibility, stability, and strength. This has been shown to reduce the risk of symptoms from arthritis.
Can I run and exercise after a discectomy?
In hospital you will be given basic exercises after your operation and be encouraged to keep mobile. Normally, you will be reviewed around 2 weeks to ensure your wound is healing. At approximately 3 weeks or once your wound is healed, you will be allowed to start physiotherapy and one to one Pilates with an appropriately trained instructor. If there are no complications, you can get on an upright exercise bike after this.
Your physiotherapist will determine when you can start running. You will need to do strength work for 6-8 weeks prior to running and will start impact work around the 8-10 week mark.
How long will it take me to recover from a discectomy?
Recovery time depends on a number of factors including your initial diagnosis, how many levels are involved, how long you have had the symptoms, and the exact nature of the procedure. It also depends on your general health.
Timeline:
- Get out of bed and walking the same day
- Go to clinic 2 weeks post operation
- At approximately week 3 rehabilitation begins
- Back to work in the office part time at 2.5 weeks post operation
- Driving at approximately 4 weeks post operation
Although many people feel symptomatic improvement in the weeks following surgery, it can take up to a year to feel the full benefits. This is how long it can take the nerve to fully recover. In some patients, the nerve will not fully recover and you may be left with some residual symptoms.
How long do I have to be in hospital for after a discectomy?
For a one or two level discectomy’s, patients stay overnight or occasionally two nights.
Will I have a big scar after a discectomy?
Often you will have a very small scar after your discectomy. More frequently, a microdiscectomy is done which means your incision is around 2 – 2.5cms. You should discuss this with your Consultant as it will depend on how many levels are being operated on and the nature of your surgery.
Will I need time off work after a discectomy?
Yes, you will normally need 2 weeks off full-time work, but this can be up to 3 weeks depending the nature of your job and surgery. Two weeks is estimated for desk based or non-manual jobs. If you have a manual job, you should discuss this with your Consultant. They will talk through your options and whether you can return to light duties.
Another factor to consider is how long your commute is, and the means of transport you use. It would be worth discussing this with your Consultant as well.
In general, you should be working from home after one week and gradually moving to part time in the office at 2.5 weeks. If you commute by public transport, this should be in off-peak hours. You can then sensibly increase your hours to full time after this, aiming for full time at 4 weeks. You will not be able to drive for four weeks following surgery so bear this in mind if you commute by car.
Education is key:
These blogs are designed to give information to everyone, however, it is important to remember that everyone is different! If you have not seen one of our therapists and have any questions about injuries, what you have read or whether this may be useful to you, please just ask. We are more than happy to help anyone and point you in the right direction. Our biggest belief is that education is key. The more you understand about your injury, illness and movement, the more you are likely to improve.